A new blood test is being developed to improve ovarian cancer diagnosis, with the potential to reduce unnecessary surgery leading to better health outcomes, saving time, stress and money for patients as well as the healthcare system.
Hudson Institute of Medical Research, funded by the Ovarian Cancer Research Foundation (OCRF), has developed a new diagnostic test for ovarian cancer, which is now being commercialised by ASX-bound Australian company Cleo Diagnostics Ltd.
Cleo will advance the availability of its cancer diagnostics platform, which is designed to eventually address all ovarian cancer detection markets with specific tests including surgical triage, recurrence, high risk, and early-stage screening. The test will now enter a development phase and undergo validation prior to clinical use.
The blood tests will be underpinned by a patented novel biomarker, CXCL10, which is produced early and at high levels by ovarian cancers, but not in non-malignant disease.
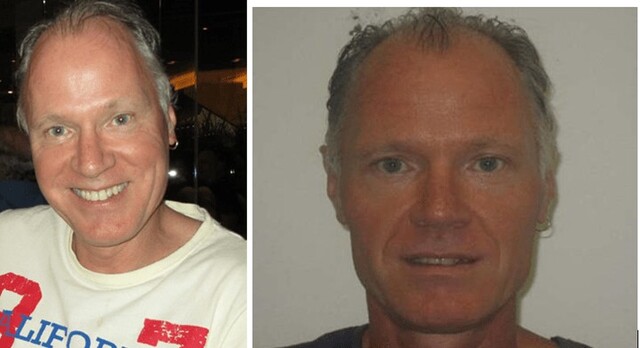
CXCL10 was first identified at Hudson Institute by Dr Andrew Stephens, who is now Cleo’s Chief Scientific Officer.
Initial clinical use will focus on the surgical triage market to improve treatment outcomes for patients with ovarian cancer, and simultaneously avoid unnecessary surgery and anxiety for women with far more common non-cancerous conditions.
Beyond surgical triage, Cleo Diagnostics will conduct further clinical trials to evaluate the effectiveness of the underlying core technology for disease recurrence following surgery and ultimately aims to develop broader screening applications in the general population.
There is no accurate and reliable detection test for ovarian cancer — a pap test does not detect ovarian cancer. Ovarian cancer is the most lethal of all cancers affecting women in Australia, and a silent killer. The current five year survival rate is 49 per cent and this has not changed substantively in 50 years.
Ovarian cancers are often indistinguishable from common, non-cancerous disease. Currently patients undergo a combined CA-125 blood test and ultrasound to provide an assessment of disease.
However, neither is sufficient for an accurate diagnosis and they are only used for surgical referral.
Invasive surgery to remove the ovaries remains the only way to definitively diagnose the presence of malignant disease.
As a result, a large proportion of women experience a cancer scare, undergoing unnecessary anxiety, trauma and invasive surgery due to the lack of accurate diagnostic technology.
The CLEO surgical Triage Test is being developed as an easy to administer blood test that accurately distinguishes benign from malignant disease without surgical intervention.
The potential benefits are significant including improved early evaluation of patients using a simple blood test, that provides an actual cancer
diagnostic assessment before surgery is considered, high specificity and sensitivity to identify cancer, allowing efficient referral of patients to an
appropriate gynaecological oncology surgeon for treatment, patients that are diagnosed with non-cancerous growths will benefit from more conservative management strategies and substantial reduction in stress and anxiety experienced by women who undergo a ‘cancer scare’ and must wait for a surgical diagnosis.
CLEO Diagnostics lead medical advisor Professor Tom Jobling said there is often a delay in sending patients to a gynaecological oncology specialist for treatment, because defining whether a growth is likely to be malignant or not before surgery is very difficult.
“This new test will help ensure that an optimal management plan can be put in place early, which will streamline the referral process and provide the best care for patients,” he said.
“This also extends to patients with benign conditions, where early identification will permit direction to more appropriate use of resources.”
Cleo Diagnostics rare planning for initial clinical triage use in 2025.